Crammed elbow to elbow around a table in a tiny basement-level Clark Center conference room, a multidisciplinary cross-section of scientists, physicians, engineers and students convened to scarf sandwiches and compare notes.
They were there that fateful Friday in 2019 because Karl Deisseroth, MD, PhD — one of Stanford Medicine’s most forward-thinking researcher-clinicians — had invited them. And lunch was on him.
“We needed a lot of sandwiches in that jam-packed little room,” recalled the D. H. Chen Professor and a professor of bioengineering and of psychiatry and behavioral sciences.
He referred to the every-few-months gatherings that typically occurred on Fridays as “clinical subgroup meetings,” but most who were invited knew them simply as “Karl’s lunches.” And for the med school’s most inquisitive minds, they were hot-ticket invitations.
Deisseroth began putting these lunches together more than a decade ago not to feed bored, hungry medical folks but to feed fires in them, foster communication and create the kind of alchemy he believed necessary for quicker medical science advances. Turns out, it worked.
In November, Deisseroth and his team of collaborators introduced a major byproduct of that bread breaking: the Human Neural Circuitry program. Stationed at a corner suite partitioned from a wing on the new Stanford Hospital’s fifth floor, the recently launched program pools the expertise of disparate brain specialists — psychiatrists, neurologists, neurosurgeons, anesthesiologists and bioengineers.
At their disposal: cutting-edge tools to measure cognitive function, a high-powered data-gathering infrastructure to process and study brain activity in real time, and experienced hospital staff to care for actual patients from within and outside the Stanford Health Care system.
What makes the program unique? There is the super-charged network speed and computational power: Data goes from the patient’s brain, transmitted by electrodes placed inside the skull or detectors on the surface, to a server across campus and back to the researchers in half a millisecond, Deisseroth said.
“There’s nothing like the real-time verbal feedback we can get from our fellow human beings.”
And there is the hybrid hospital room/research setting that includes a small bio lab where living cells coming straight from a patient’s brain can be instantly analyzed, with full consent of the participants. The cells come from clinically useful electrodes that were placed for medical care and would otherwise have been discarded. A graduate student in Deisseroth’s lab at the time — Sam Vesuna, MD, PhD, currently a resident in Stanford’s psychiatry program — heads up that bio lab analysis.
“This area of the hospital is set up for medical care of patients who have just had brain surgery and have electrodes implanted deep in their brains,” Deisseroth said. “It’s state-of-the-art medicine, but it also provides an amazing source of real-time data from the brain of a human beings.”
Another asset this setup offers: human communication. Alongside the electrophysiological and cellular analyses, people provide real feedback — whether prompted by an artful psychiatric interview or just natural conversation. Mice and other animals have aided neuroscience understanding, but the limitations are obvious.
“There’s nothing like the real-time verbal feedback we can get from our fellow human beings,” Deisseroth said.
If you build it
Deisseroth, the program’s creator and director, is both a practicing psychiatrist, mostly treating patients with depression and autism, and one of the world’s leading neuroscientists and bioengineers. With a foothold in the research and clinical worlds, he was an ideal person to broker the launch of the program.
The goal? To study the human brain in a fashion previously attempted only in animal models. In time, the collaborators believe, discoveries made through the program will lead to new therapies for all manner of neuropsychiatric disorders — conditions ranging from depression and anxiety to epilepsy and Parkinson’s to obsessive-compulsive disorder and autism to eating disorders and schizophrenia.
The Human Neural Circuitry program is an extension of the lunches where the silo-busting began. Those helping Deisseroth run it — Paul Nuyujukian, MD, PhD, an assistant professor of bioengineering and of neurosurgery; Carolyn Rodriguez, MD, PhD, a professor of psychiatry and behavioral sciences; and Vivek Buch, MD, assistant professor of neurosurgery — represent historically disparate fields of brain science, but each has joined with Deisseroth for many meetings every week over the past two years to help build the program.
‘A flash of light’
Deisseroth caught a glimpse of this future at that standing-room-only lunch in 2019 that sparked the program’s creation. During the discussion, a member of Deisseroth’s team (graduate student Isaac Kauvar, who was working with Vesuna) shared results of their mouse study of dissociation — a mental disconnection of emotion from sensations of the body. A neurosurgeon (professor of neurosurgery Jaimie Henderson, MD) chimed in that he had performed surgery on an epilepsy patient experiencing spontaneous dissociation.
Eyebrows immediately raised around the table; intrigued smiles formed. Why couldn’t those two studies be synergized, with resulting insights made many more times powerful?
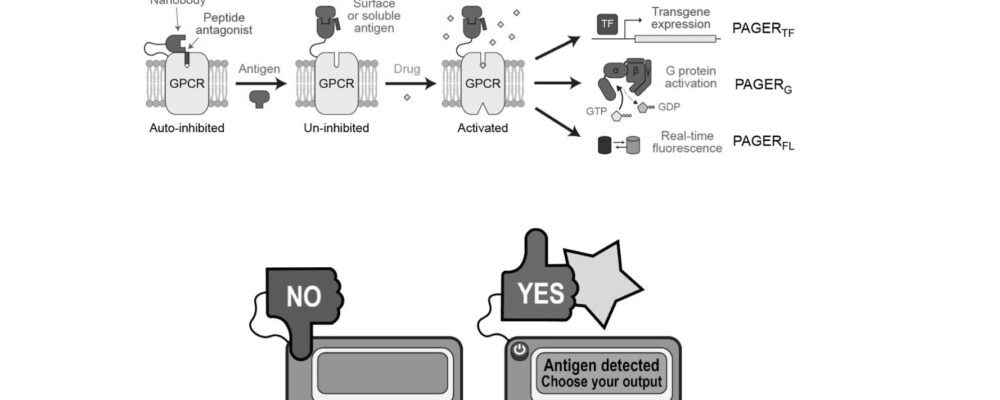
From here, Deisseroth, Kauvar and Vesuna, along with several colleagues, launched their study: By using comparative data from laboratory mice and a patient at the Stanford Comprehensive Epilepsy Program suffering from a severe seizure disorder, the team was able to implicate a particular kind of activity of certain sets of cells in dissociation — both in human and mouse. The team — which also included Henderson, Nuyujukian and Josef Parvizi, MD, PhD, professor of neurology, who had treated the initial patient with Henderson — published their results in 2020 in Nature.
“This program makes clear the irreplaceable value of just getting together and talking over lunch.”
Their reveal of this physical underpinning for a previously unexplainable mind state became the crucial proof of concept for a collaborative program combining brain studies in animals and humans.
After the success of this effort, Deisseroth began rallying stakeholders to create the broader program, meeting with hospital and medical school leaders, space planners, nurses, physicians, clinical trial staff, and research protocol committees, along with Nuyujukian, Rodriguez and Buch.
Many years — and many conversations — later, the Human Neural Circuitry program was born. Several studies have been launched through the program, with more on the way — all using the powerful tools of modern science inside a clinical setting with real patients: a dream come true for those seeking to understand the inner workings of the brain.
“This program makes clear,” Deisseroth said, “the irreplaceable value of just getting together and talking over lunch.”
“Stanford University, officially Leland Stanford Junior University, is a private research university in Stanford, California. The campus occupies 8,180 acres, among the largest in the United States, and enrols over 17,000 students.”
Please visit the firm link to site