Seeing what’s going on inside a body is never easy. While technologies like CT scans, X-rays, MRIs, and microscopy can provide insights, the images are rarely completely clear and can come with side effects like radiation exposure.
But what if you could apply a substance on the skin, much like a moisturizing cream, and make it transparent, without harming the tissue?
That’s what Stanford scientists have done using an FDA-approved dye that is commonly found in food, among several other light-absorbing molecules that exhibit similar effects. Published in Science on Sept. 5, the research details how rubbing a dye solution on the skin of a mouse in a lab allowed researchers to see, with the naked eye, through the skin to the internal organs, without making an incision. And, just as easily as the transparency happened, it could be reversed.
“As soon as we rinsed and massaged the skin with water, the effect was reversed within minutes,” said Guosong Hong, assistant professor of materials science and engineering and senior author on the paper. “It’s a stunning result.”
Absorption reduces scattering of light
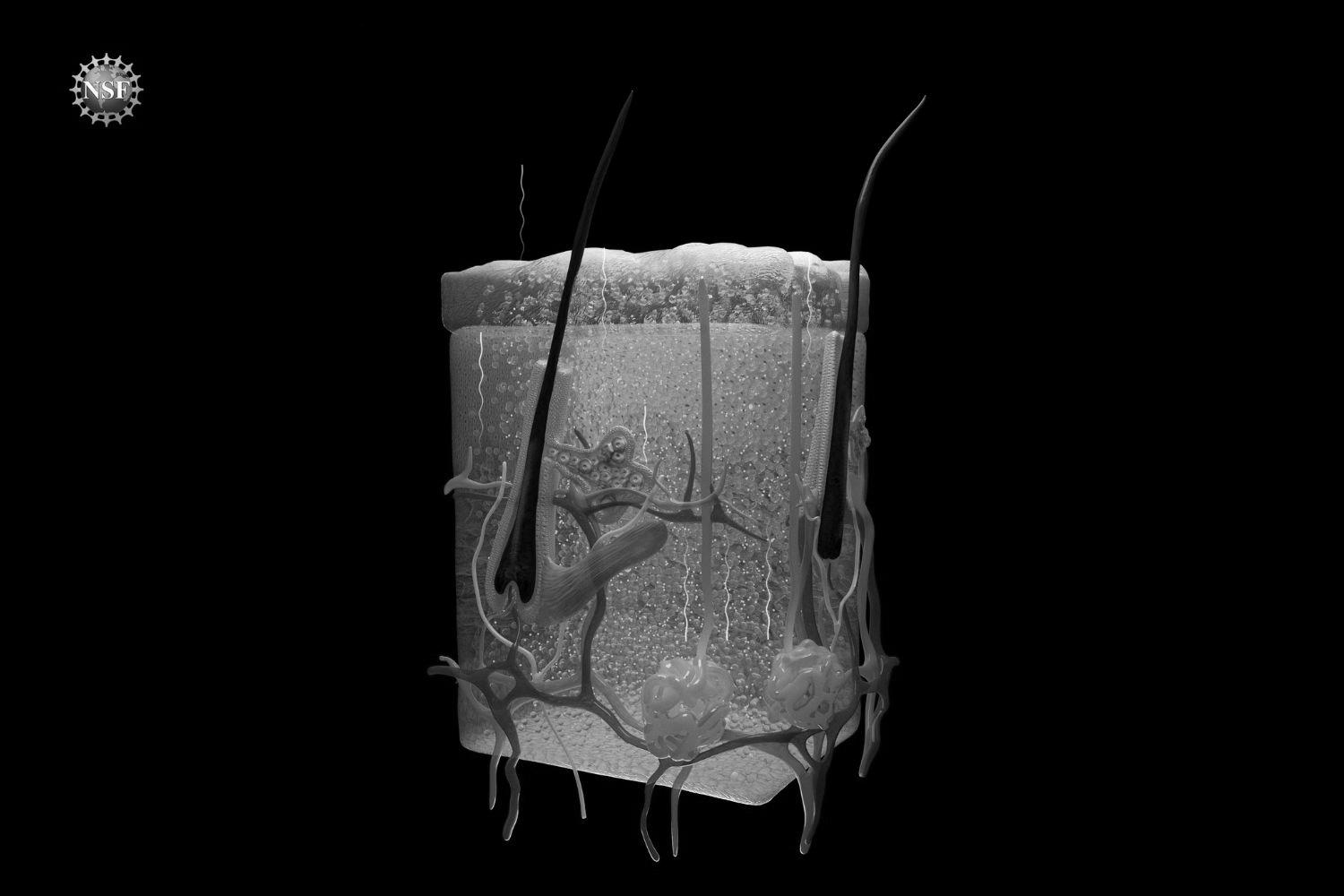
When light waves strike the skin, the tissue scatters them, making it appear opaque and non-transparent to the eye. This scattering effect arises from the difference in the refractive indices of different tissue components, such as water and lipids. Water usually has a much lower refractive index than lipids in the visible spectrum, causing visible light to scatter as it goes through tissue containing both.
To match the refractive indices of different tissue components, the team massaged a solution of red tartrazine – also known as the food dye FD&C Yellow 5 – onto the abdomen, scalp, and hindlimb of a sedated mouse. The skin turned red in color, indicating that much of the blue light had been absorbed due to the presence of this light-absorbing molecule. This increase in absorption altered the refractive index of the water at a different wavelength – in this case, red. As a result of the absorption of the dye, the refractive index of water matches that of lipids in the red spectrum, leading to reduced scattering and making the skin appear more transparent at the red wavelength.
This research is a new application of decades-old equations that can describe the relationship between absorption and refractive index, called the Kramers-Kronig relations. In addition to this food dye, several other light-absorbing molecules have demonstrated similar effects, thereby confirming the generalizability of the underlying physics behind this phenomenon.
Researchers were able to see, without special equipment, the functioning internal organs, including the liver, small intestine, cecum, and bladder. They were also able to visualize blood flow in the brain and the fine structures of muscle fibers in the limb. The mouse’s beating heart and active respiratory system indicated that transparency was successfully achieved in live animals. Furthermore, the dye didn’t permanently alter the subject’s skin, and the transparency disappeared as soon as the dye was rinsed with water.
The researchers believe this is the first non-invasive approach to achieving visibility of a mouse’s living internal organs.
“Stanford is the perfect place for such a multifaceted project that brings together experts in materials science, neuroscience, biology, applied physics, and optics,” said Mark Brongersma, professor of materials science and engineering and co-author on the paper. “Each discipline comes with its own language. Guosong and I enjoyed taking each other’s courses on neuroscience and nanophotonics to better appreciate all the exciting opportunities.”
The potential future of ‘clear’ tissue
Right now, the study has only been conducted on an animal. If the same technique could be translated to humans, it could provide a range of biological, diagnostic, and even cosmetic benefits, Hong said.
For example, instead of through invasive biopsies, melanoma testing could be done by looking directly at a person’s tissue without removing it. This approach could potentially also replace some X-rays and CT scans, and make blood draws less painful by helping phlebotomists easily find veins. It could also improve services like laser tattoo removal by helping to focus laser beams precisely where the pigment is below the skin.
“This could have an impact on health care and prevent people from undergoing invasive kinds of testing,” said Hong. “If we could just look at what’s going on under the skin instead of cutting into it, or using radiation to get a less than clear look, we could change the way we see the human body.”
Other Stanford co-authors include Betty Cai, member of the Department of Materials Science Engineering; Zihao Ou, Carl H. C. Keck, Shan Jiang, Kenneth Brinson Jr, Su Zhao, Elizabeth L. Schmidt, Xiang Wu, Fan Yang, Han Cui, and Shifu Wu, who are also with the Department of Materials Science Engineering and Wu Tsai Neurosciences Institute; Yi-Shiou Duh of the Department of Physics and Geballe Laboratory for Advanced Materials; Nicholas J. Rommelfanger of the Wu Tsai Neurosciences Institute and Department of Applied Physics; Wei Qi and Xiaoke Chen of the Department of Biology; Adarsh Tantry of the Wu Tsai Neurosciences Institute and Neurosciences IDP Graduate program; Richard Roth of the Department of Neurosurgery; Jun Ding of the Department of Neurosurgery and Department of Neurology and Neurological Sciences; and Julia A. Kaltschmidt of the Wu Tsai Neurosciences Institute and Department of Neurosurgery.
This work was supported by the National Institutes of Health, National Science Foundation, Air Force, Beckman Technology, Rita Allen Foundation, Focused Ultrasound Foundation, Spinal Muscular Atrophy Foundation, Pinetops Foundation, Bio-X Initiative of Stanford University, Wu Tsai Neuroscience Institute, Knight-Hennessy, and U.S. Army Long Term Health Education and Training program.
Disclaimer: The technique described above has not been tested on humans. Dyes may be harmful. Always exercise caution when handling dyes – do not consume them, apply them to people or animals, or misuse them in any way.
“}”>
For more information
*:last-child]:su-mb-0″ readability=”46.426058631922″>
Other Stanford co-authors include Betty Cai, member of the Department of Materials Science Engineering; Zihao Ou, Carl H. C. Keck, Shan Jiang, Kenneth Brinson Jr, Su Zhao, Elizabeth L. Schmidt, Xiang Wu, Fan Yang, Han Cui, and Shifu Wu, who are also with the Department of Materials Science Engineering and Wu Tsai Neurosciences Institute; Yi-Shiou Duh of the Department of Physics and Geballe Laboratory for Advanced Materials; Nicholas J. Rommelfanger of the Wu Tsai Neurosciences Institute and Department of Applied Physics; Wei Qi and Xiaoke Chen of the Department of Biology; Adarsh Tantry of the Wu Tsai Neurosciences Institute and Neurosciences IDP Graduate program; Richard Roth of the Department of Neurosurgery; Jun Ding of the Department of Neurosurgery and Department of Neurology and Neurological Sciences; and Julia A. Kaltschmidt of the Wu Tsai Neurosciences Institute and Department of Neurosurgery.
This work was supported by the National Institutes of Health, National Science Foundation, Air Force, Beckman Technology, Rita Allen Foundation, Focused Ultrasound Foundation, Spinal Muscular Atrophy Foundation, Pinetops Foundation, Bio-X Initiative of Stanford University, Wu Tsai Neuroscience Institute, Knight-Hennessy, and U.S. Army Long Term Health Education and Training program.
Disclaimer: The technique described above has not been tested on humans. Dyes may be harmful. Always exercise caution when handling dyes – do not consume them, apply them to people or animals, or misuse them in any way.
“Stanford University, officially Leland Stanford Junior University, is a private research university in Stanford, California. The campus occupies 8,180 acres, among the largest in the United States, and enrols over 17,000 students.”
Please visit the firm link to site