As wildfires continue to rage across the Los Angeles area, their toll on lives, homes, and natural landscapes is undeniable. Less obvious are the health impacts, such as respiratory issues caused by smoke inhalation and mental health strains of evacuation and loss, that could stretch far beyond the burn zone and linger for years to come.
Stanford researchers are working to uncover the full scope of wildfire-related health risks and how public health strategies can mitigate them. Below, four Stanford experts spanning the fields of environmental science, medicine, and public health discuss what we know about wildfires’ health impacts, what remains a mystery, and how communities can better protect themselves from the increasingly common threat.
Lisa Patel, a clinical associate professor of pediatrics in the Stanford School of Medicine, is the lead author of Climate Resilient Schools: A Call to Action, a report that details wildfire impacts on children’s health and recommends policy solutions. Sharon Chinthrajah, an associate professor of medicine and pediatrics, studies allergies and asthma. Marshall Burke, an associate professor in the Stanford Doerr School of Sustainability, studies air quality impacts to human health and recently published a preprint study showing how wildfire smoke has single-handedly set back progress on clean air in the U.S. Jessica Yu, a research scientist at the Stanford Woods Institute for the Environment’s Climate and Energy Policy Program, studies the intersection of human and planetary health, with a focus on the public health impacts of wildfire smoke. (See more Stanford experts on wildfires.)
Is wildfire smoke more dangerous than other forms of air pollution? How can we gauge the danger, and protect against it?
Burke: The data pretty clearly say that there is no safe level of exposure to wildfire smoke: the more exposure we get, the worse a range of health outcomes. The data also pretty clearly show that our notion of sensitive groups should probably be greatly expanded. In addition to kids, elderly populations, or anyone else with preexisting conditions, like asthma, we need to think about populations like pregnant people whose birth outcomes can be substantially affected by exposure. Portable indoor filtration is often the best option for many households, and well-fitting N95 masks can help when outside.
Patel: We estimate that wildfire smoke is about 10 times as toxic as the regular air pollution we breathe from the burning of fossil fuels. Given the toxicity of wildfire smoke and that we can expect children to be exposed to these toxic events more often, I think it’s best to err on the side of caution. Children are a sensitive population and should be limiting their time outdoors during poor air quality days. Schools need to have filtration systems in place to keep indoor air quality clean for students, whether that is HVAC systems or portable air cleaners.
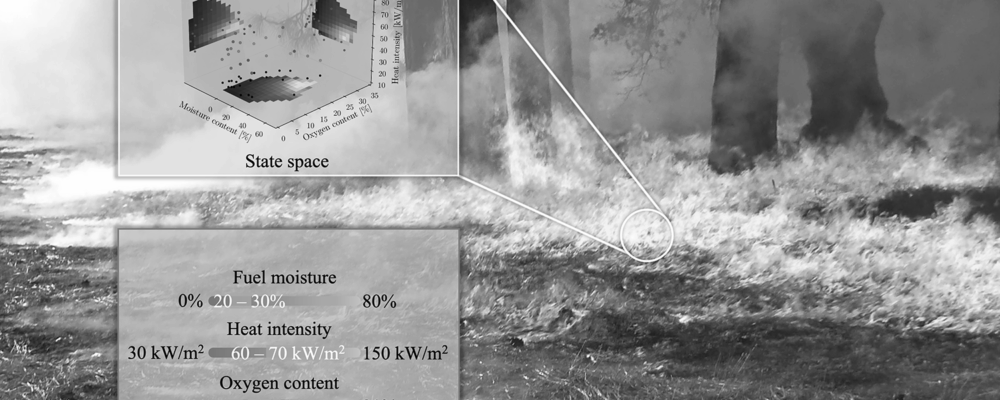
Yu: Wildfire smoke contains a variety of pollutants, and its composition depends on factors such as the type of fuel being burned, such as vegetation and housing materials, the intensity of the fire, and atmospheric conditions. These factors can lead to the release of fine particulate matter, harmful gases, volatile organic compounds, and toxic substances, like benzene and heavy metals. Fine particulate matter from wildfire smoke is particularly dangerous because it can penetrate deep into the lungs and enter the bloodstream, potentially causing damage to multiple body systems, including the cardiovascular and nervous systems.
How could repeated exposure to wildfire smoke influence the development or exacerbation of respiratory conditions in children? Are there any counterintuitive findings regarding susceptibility or resilience among different pediatric populations?
Patel: Acutely, we see more children showing up in our emergency room with asthma, wheezing, bronchitis, and pneumonia. While we don’t know long-term outcomes for what these repeated exposures mean for children, each new study that comes out should increase our concern. Studies that follow children 2-4 years after exposure to smoke form large wildfires show reduced lung function, increased antibiotic use, and increased healthcare utilization.
Yu: Infants breathe more air per unit of body weight than adult, and toxicological studies indicate that the respiratory system continues to develop until around 21 years of age. This underscores why pediatric populations are particularly vulnerable to adverse health outcomes from wildfire smoke. However, it’s important to recognize that the toxicological impacts of wildfire smoke on developing respiratory systems extend beyond young children to include adolescents, teens, and young adults.
Chinthrajah: Schools and outdoor extracurricular programs, like sports, are using AQI thresholds to determine when to limit exposure and shuttle kids indoors. However, with repeated exposures, we need to examine these approaches to make sure we are truly limiting exposure over time. Children with respiratory conditions, such as asthma, are even more susceptible.
What is the role of climate change in recent wildfire activity and smoke trends?
Burke: Climate change, and in particular increasing fuel aridity brought about by hotter temperatures and variable rainfall, is playing a central role in the recent rapid increase in wildfire activity and smoke exposure throughout the US. It is certainly not the only factor, but is substantially amplifying the risk brought about by other factors, which include a century of fire suppression that has left abundant fuels in our wildlands, as well as increased human construction and activity in the wildland-urban interface. We can say with strong confidence that climate change has made these events much more likely and much more severe.
Studies indicate that individuals in wealthier areas tend to seek more information and take protective actions during wildfire smoke events compared to those in lower-income neighborhoods. What might this imply for public health interventions?
Patel: We need to make sure we are accessing multiple channels of communication and in multiple languages so that people receive information in an appropriate and timely way. Some health systems are starting to utilize opt-in alerts for threats like extreme heat or poor air quality in which vulnerable patients receive text communications to take appropriate precautions. As these threats worsen, we need to think more about what health systems can do to better reach patients who are vulnerable.
“Stanford University, officially Leland Stanford Junior University, is a private research university in Stanford, California. The campus occupies 8,180 acres, among the largest in the United States, and enrols over 17,000 students.”
Please visit the firm link to site